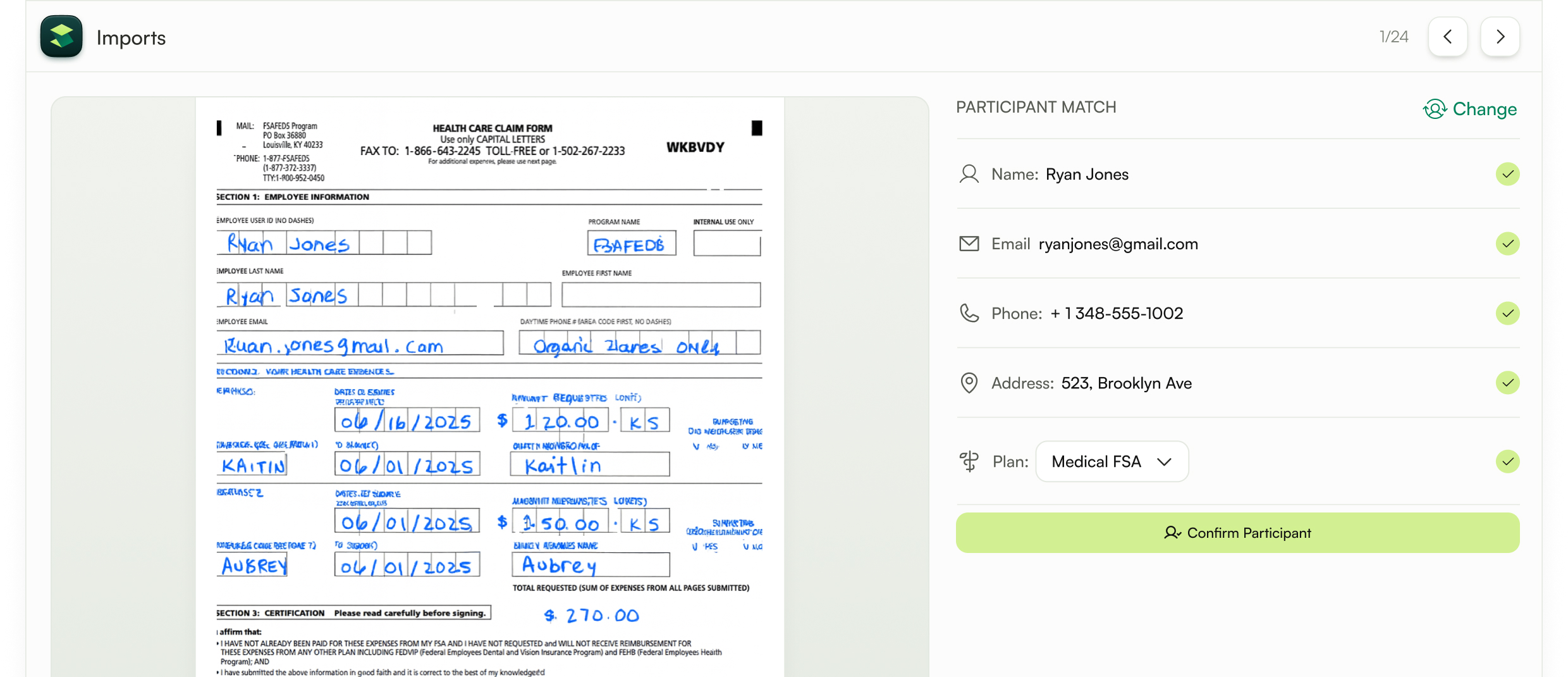
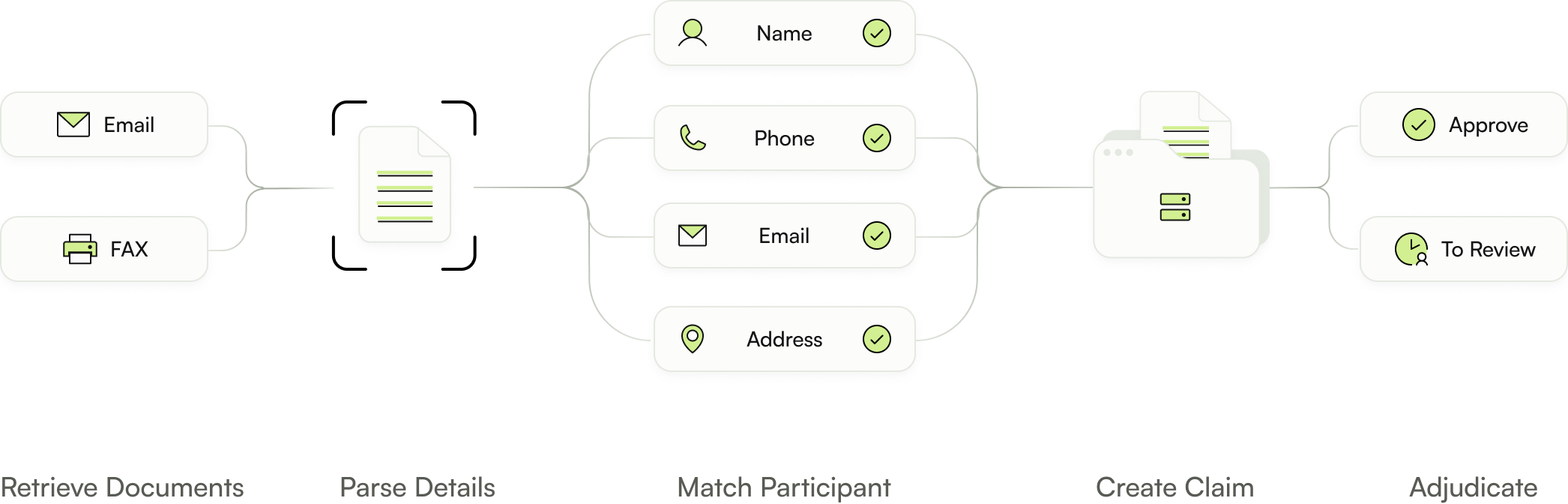
From inbox to adjudication in minutes
Participants still send claims in every possible format, which slows your team down. Silver accepts them all, including email and faxes, and converts them into claims ready to be adjudicated.
Book a Demo














.png)
.png)
.png)
Schedule a demo and discover how Silver can supercharge your claims workflows. Faster decisions, fewer errors, bigger savings.
